Hospitals are the single largest category of healthcare expenses nationally, accounting for about 1/3 of all healthcare costs.A recent summary of data from the Organization for Economic Cooperation and Development by the Commonwealth Fund shed light on realities I believe many change advocates are unaware of.
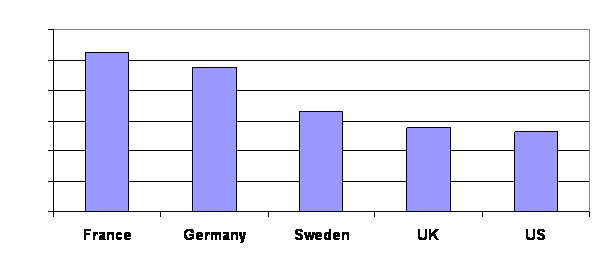
Imagine you were on a panel charged to reduce the overall cost of hospitalizations. Obviously, the first change would be to strengthen family medicine to reduce the demand in the first place. After that, here are some international comparisons to consider. One comparison of international hospital data looks like this:
Another comparison is:
Another is:
If you were on this panel, which area would you target for reform? If you said the third one presented here, it would be logical, but it is not what you commonly here from CMS and other supposed health economic experts.
Here are the comparisons with their data:

The only hospital cost reform I keep hearing about is reducing length of stay, readmissions, and admissions in the first place. As you can see, the U.S. actually does pretty well in the areas of the total number of days Americans spend in the hospital each year and the average time they spend in the hospital when they get sick.
The managed care/HMO era of the 1990s ultimately pitted many groups against each other, particularly hospitals vs. insurance companies. The hospitals won. Bolstered by their histories of being part of communities for over 100 years in many cases, they convinced the public and the payers that the nasty out-of-state insurance companies should be banished so the hospitals could survive. Of course, the insurance companies absolutely deserved heaps of derision piled on them. But the unintended negative consequence is that there was left no force to moderate hospital costs.
I have kept an eye on this issue since I started writing my book. I must say there is an extreme dearth of literature explaining the causes of the huge disparity between hospital costs in the U.S. compared to the rest of the developed world. Is it just an accounting trick – that hospitals in Europe have more of their fixed costs covered by national budgets – therefore the gap is not nearly as wide as it seems? I doubt it, but there is almost no scholarship digging into the details.
So in the absence of real evidence, here is my speculation on what is excessive in U.S. hospitals and must be cut back to achieve lower hospitalization costs (in no particular order):
- Too much spent on advertising and marketing
- Too much spent on marble counter tops and gold swan faucets
- Too much spent on layers of administration
- Too much spent on technology, especially:
- The cardiology suite
- Gamma knives
- MRIs
- PET scans
- The ICU (fancy vents and monitors, e.g.)
- Too many people running around filling out Joint Commission reports
- Too many people running around measuring a litany of outcome measures and writing quality reports
- Too many nurses spending too much time documenting patient care minutiae
Also, I think the hospitals’ claims that they have to charge so much to take care of uninsured treatment costs is exaggerated.
I could be wrong. I’ve been wrong before. But I’d love to see people who understand hospital financing in greater detail than I do shed more light on another example of extraordinary U.S. healthcare waste.






Great post. I took the liberty of reposting this on Crackinghealthcosts.com. Hope you don’t mind.
Please keep them coming.
Cheers,
Tom Emerick
Tom,
I’m glad you liked the post. Re-post it to your heart’s content.
Richard